Tetralogy of Fallot Repair in a 17-Year-Old Male
Jenna Lehn
HPI
A 17 y.o. male with a past medical history of unrepaired Tetralogy of Fallot (TOF), anorectal malformation s/p colostomy at birth, unilateral hearing loss, and chronic malnutrition presented for pre-operative examination for TOF repair. TOF and anorectal malformation were diagnosed at birth. He recently moved to the U.S. from the Philippines and was unable to obtain resources for operative repair while in the Philippines and has only been taking carvedilol.
Patient had a recent hospitalization for chronic malnutrition and refeeding syndrome. Pelvic MRI revealed a tethered cord and horseshoe kidney. Denies history of urinary retention, UTIs, or numbness or tingling in the lower extremities. Neurosurgery and nephrology follow-up were scheduled for 6 months. Anorectal malformation at birth was fixed with a posterior sagittal anorectoplasty followed with rectal dilations in the Philippines. The final colostomy takedown was never performed, and irritation of scar tissue during hospitalization was followed by general surgery with discussion of colostomy take-down follow-up in 6 months.
The patient presented for surgical repair of TOF pre-op clearance. He reported multiple daily episodes of significant cyanosis and chronic exercise intolerance since childhood. He could not run and has had difficulty with ambulation, requiring a wheelchair at times. He rests, lies down, or uses squatting to relieve symptoms. Physical exam showed significant clubbing of the upper and lower extremities in addition to short stature and small frame.
Vitals showed a heart rate of 68 and SpO2 at 75%. Pre-operative labs were ordered and CBC showed elevated hemoglobin at 23.6 g/dL and hematocrit at 76.9%, which was indicative of chronic hypoxemia-related polycythemia. VACTERL and other genetic studies were ordered and came back negative.
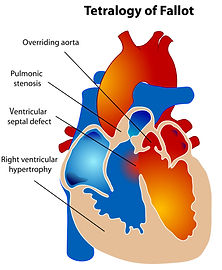
Previous echocardiogram report from the Philippines confirmed TOF with pulmonary stenosis, right ventricular hypertrophy, an overriding aorta, and a large anterior malalignment ventricular septal defect (VSD) with bidirectional shunting. Follow-up cardiac CT in previous hospitalization for malnutrition confirmed TOF.
TOF Repair
A midline sternotomy and cardiopulmonary bypass was established, and the right ventricular outflow tract was reconstructed with resection of muscle bundles to fix the hypertrophy. VSD patch closure was completed and the hypoplastic pulmonary valve was replaced.
Profound hypotension required resuscitation with blood products, vasopressors, and methylene blue. Hemostasis was achieved after prolonged efforts due to complications from chronic hypoxemia and polycythemia. Postoperative transesophageal echo showed an intact VSD patch, no right ventricular outflow tract obstruction, and an intact pulmonary valve.
Patient was treated with an appropriate pain regimen and cefazolin post-operatively. Daily aspirin was initiated, and patient saw marked improvements in activity tolerance on discharge.
Discussion
This case highlights the complexity of managing a delayed TOF repair with significant comorbidities. Tetralogy of Fallot is a congenital heart defect consisting of a combination of pulmonary stenosis, right ventricular hypertrophy, a ventricular septal defect, and an overriding aorta. Treatment is always surgical and typically performed in the first year of life. This particular case is unique in that surgery was not able to be performed until the patient was 17 years of age. This resulted in the patient’s severe symptoms of chronic activity intolerance, cyanosis, polycythemia, and short stature. Patients commonly present with “tet spells,” which are sudden development of cyanosis in the lips, face, and extremities that are relieved by stopping physical activity or squatting. Squatting increases the peripheral vascular resistance followed by decreased right to left shunting across the VSD.